The Impact on Inflammation
Introduction
Chronic inflammation initiates through a complex interplay of cellular and molecular mechanisms within the body. It often begins as a response to harmful stimuli, such as pathogens, toxins, or tissue damage. When the immune system detects these threats, it releases a cascade of chemical messengers called cytokines, which attract immune cells to the affected area. These immune cells, including macrophages and neutrophils, release additional cytokines, initiating a process known as the inflammatory response. While acute inflammation is a necessary and beneficial defense mechanism for healing, chronic inflammation occurs when this response becomes dysregulated and persists over an extended period.
Chronic Inflammation is now recognized as a major contributor to many chronic health conditions, including heart disease, diabetes, cancer, and autoimmune disorders. Chronic inflammation can also contribute to the aging process, as it damages cells and tissues throughout the body. One of the primary ways in which chronic inflammation contributes to poor health is by inducing oxidative stress. Inflammatory processes trigger the production of free radicals, which are unstable molecules capable of causing harm to cells and DNA. Prolonged exposure to this damage can contribute to the development of chronic diseases and accelerate the aging process.
How does chronic inflammation start?
Chronic inflammation can be fueled by various factors, including processed foods, sedentary lifestyle, obesity, stress, and environmental toxins. Over time, the continuous production of pro-inflammatory molecules, such as cytokines and reactive oxygen species, leads to tissue damage and can contribute to the development of chronic disease.
- Persistent Infections or Autoimmune Reactions: Long-term exposure to pathogens or an autoimmune response (where the body mistakenly attacks its cells) can lead to chronic inflammation.
- Lifestyle Factors: Unhealthy lifestyle choices such as poor diet high in processed foods, lack of physical activity, chronic stress, inadequate sleep, and habits like smoking and excessive alcohol consumption can contribute to chronic inflammation.
- Chronic Diseases: Certain chronic conditions like obesity, diabetes, heart disease, and some types of cancer are associated with higher levels of inflammation.
- Gut Health and Microbiome Imbalance: An imbalance in the gut microbiome, also known as dysbiosis, can lead to an increase in gut permeability (or “leaky gut”), allowing bacteria and toxins to cross into the bloodstream, which can trigger chronic inflammation.
- Genetic Factors: Certain genetic factors can predispose individuals to heightened inflammatory responses.
Arachidonic acid
Arachidonic acid is a fatty acid that is stored within the cell membrane of many cells in the body. When a cell is activated by an external stimulus, such as an injury or infection, arachidonic acid is released from the cell membrane by an enzyme called phospholipase A2.
Once released, arachidonic acid can be metabolized by several enzymes to produce a range of bioactive compounds, including leukotrienes, prostaglandins, and thromboxanes. These compounds are collectively known as eicosanoids and play important roles in a range of physiological processes, including inflammation, pain, and blood clotting.
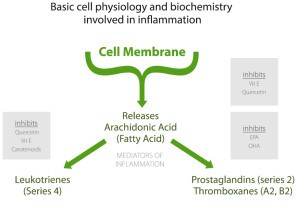
Chronic inflammation can cause a dysregulation of the arachidonic acid pathway. When inflammation persists over a prolonged period, the increased production of these compounds can lead to an imbalance in the body’s immune response and contribute to negative health outcomes.
Gut Microbiome
Chronic inflammation can significantly alter the gut microbiome, the diverse community of microorganisms living in our intestines. The connection between inflammation and the gut microbiome is bidirectional, meaning that not only can an imbalanced gut microbiome contribute to inflammation, but chronic inflammation can also disrupt the gut microbiome.
This disruption of the balance of the gut microbiome leads to a state known as dysbiosis. Dysbiosis refers to a shift in the composition of the microbiome, typically characterized by a decrease in beneficial bacteria and an increase in potentially harmful bacteria. This change can perpetuate inflammation, leading to a cycle of inflammation and dysbiosis.
We will discuss gut health in greater detail in the next chapter.
Insulin Resistance
Chronic inflammation can contribute to insulin resistance by increasing the production of pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6). These cytokines can interfere with insulin signaling and disrupt glucose uptake by the cells, leading to high blood sugar levels and insulin resistance.
When the body is in a state of chronic inflammation, it can lead to increased lipid oxidation and breakdown of stored fat. This results in the accumulation of fatty acids in the liver and skeletal muscle, which interferes with insulin signaling between cells. We will also go into more detail with this process when we discuss hormones.
Anti-inflammatory foods
Adopting an anti-inflammatory approach can help mitigate chronic inflammation by focusing on whole, unprocessed foods and avoiding potential triggers, thus promoting overall health and well-being.
Healthy fats and numerous micronutrients from an anti-inflammatory diet have been shown to reduce inflammation, which can help reduce the risk of chronic disease. A key mechanism through which this approach achieves inflammation reduction is by balancing the intake of omega-6 and omega-3 fatty acids. Omega-6 fatty acids, commonly found in processed foods, have been associated with promoting inflammation when consumed excessively. Conversely, sources abundant in omega-3 fatty acids, such as wild-caught fish and nuts, have demonstrated anti-inflammatory effects. By adopting a diet rich in omega-3s and limiting omega-6s, individuals can effectively decrease their susceptibility to chronic inflammation.
Foods to Increase
- Berries: Berries, such as strawberries, blueberries, and raspberries, are rich in antioxidants and phytonutrients that have anti-inflammatory properties.
- Leafy greens: Leafy greens, such as spinach and kale, are rich in vitamins, minerals, and phytonutrients that have anti-inflammatory properties.
- Fatty fish: Fatty fish, such as salmon and mackerel, are rich in omega-3 fatty acids, which have been shown to have anti-inflammatory effects.
- Nuts and seeds: Nuts and seeds, such as almonds and chia seeds, are rich in healthy fats and antioxidants that have anti-inflammatory properties.
- Ginger and turmeric: Ginger and turmeric are spices that have long been used for their anti-inflammatory properties. They contain compounds that have been shown to have a positive impact on reducing chronic inflammation in the body.
- Cruciferous vegetables: Vegetables such as broccoli and cauliflower contain compounds that have been shown to have anti-inflammatory effects.
Anti-inflammatory phytonutrients
- Flavonoids: Flavonoids are a group of phytonutrients found in a variety of fruits, vegetables, and other plant-based foods. They have been shown to have anti-inflammatory properties and to protect against oxidative stress.
- Carotenoids: Carotenoids are a group of phytonutrients found in brightly colored fruits and vegetables, such as carrots and sweet potatoes. They have been shown to have anti-inflammatory effects and to support eye health.
- Resveratrol: Resveratrol is a phytonutrient found in red wine, grapes, and other plant-based foods. It has been shown to have anti-inflammatory properties and to protect against oxidative stress.
- Curcumin: Curcumin is a phytonutrient found in turmeric. It has been shown to have anti-inflammatory properties and to protect against oxidative stress.
- Indoles: Indoles are a group of phytonutrients found in cruciferous vegetables, such as broccoli and cauliflower. They have been shown to have anti-inflammatory effects and to protect against oxidative stress.
- Terpenes: Terpenes are a group of phytonutrients found in a variety of plant-based foods. They have been shown to have anti-inflammatory properties and to protect against oxidative stress.
Quick Summary
Chronic inflammation can lead to negative health effects and contribute to the development of various chronic health conditions. It can cause dysregulation of the arachidonic acid pathway, disrupt the gut microbiome, and contribute to insulin resistance. Consuming anti-inflammatory foods, such as berries, leafy greens, fatty fish, nuts and seeds, ginger and turmeric, and cruciferous vegetables, can help to reduce chronic inflammation. Additionally, consuming phytonutrients like flavonoids, carotenoids, resveratrol, curcumin, indoles, and terpenes, which are found in a variety of plant-based foods, can also have anti-inflammatory effects and protect against oxidative stress.


