We live in a world in which many people are feeling the effects of stress more than ever.
The human body is equipped with a sophisticated stress response system that enables us to immediately react to whatever stressful stimuli we are exposed to. However, when stress becomes chronic, this same system can also cause wear and tear on the body when its constantly being stimulated.
Most people are aware that long-term stress can lead to health problems but may not readily recognize the signs and symptoms of this wear and tear or make the connection that these are stress-related.
How the Stress Response System Works
Our stress response system is controlled by communications between the hypothalamus, pituitary, and adrenal glands and is called the hypothalamus-pituitary-adrenal axis or HPA axis for short. The HPA axis also influences important body processes such as blood sugar balance and insulin sensitivity.
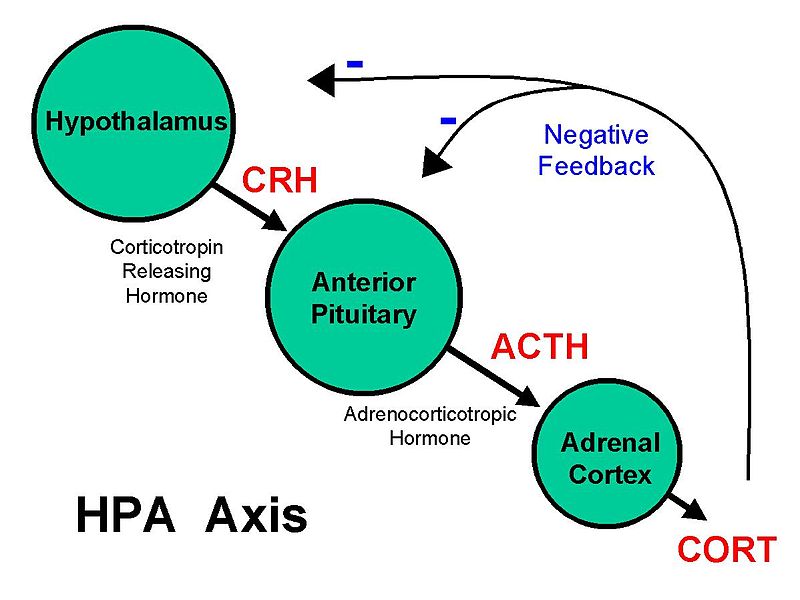
When our brain detects stress, signals are sent to the adrenal glands that stimulate the release of catecholamines (epinephrine and norepinephrine), mineralocorticoids (aldosterone), and glucocorticoids (cortisol and DHEA-S) which result in a series of physiological reactions in the body to prepare us to respond.
Heart rate and blood pressure increases. The liver converts glycogen to glucose which is released into circulation raising our blood sugar. Other physiological changes help us become more alert and energized while also decreasing activity in the body that is not needed during a stressful event, such as slowing digestive, thyroid, metabolic, and immune functions.
This puts us into “fight-or-flight” mode giving us greater mental and physical ability to deal with the emergency.
Once the emergency is over, our stress response system deactivates and we return to a normal state of being.
This system works remarkably well potentially protecting us from acute stressful situations, such as giving us increased energy to escape from a burning building or to defend against a predator.
Fortunately for most of us, we are not faced with these types of life-threatening emergencies often, however, our stress response system is repeatedly triggered multiple times per day due to the stressors of modern life that we routinely experience. Many of us live fast-paced lives with constant access to email and text messaging with very little downtime to unwind and recharge.
Getting stuck in traffic on the way to an important meeting, relationship difficulties, financial struggles, and juggling family responsibilities along with career pressures are daily stressors for many people. This chronic stress puts us into frequent “fight-or-flight” mode which creates HPA axis dysfunction and can eventually result in a myriad of health consequences.
What Triggers Stress-Induced HPA Axis Dysfunction?
Chronic stress over time triggers HPA axis dysfunction. While we often associate stress with mental or emotional stress, it’s important to note that the body responds to all types of stress.
What this means, is that in addition to mental or emotional stress, stressors can be physical or environmental in nature. For example, the body is stressed when we are sleep deprived or are habitually overtraining with exercise or have a recurring infection/illness such as bronchitis or pneumonia. Stressors can also be a high-pressure job or an unhappy marriage.
More examples of what can be stressful to the body:
- Autoimmune disease
- Blood sugar imbalance
- Dehydration
- Infection
- Inflammation (from leaky gut, viruses, blood sugar imbalance, chronic disease)
- Oxidative stress
- Certain medications
- Nutrient insufficiencies
- Toxin burden
- Skipping meals
- Inadequate sleep
- Nutrient-poor diet
With chronic stress, we don’t have a chance to build up our metabolic reserves and this prevents us from being resilient to the next stressor that comes our way. This is when we start feeling less energetic (from less ATP production) and develop more oxidative stress, leading to a bunch of different symptoms.
Signs and Symptoms of HPA Axis Dysfunction
The collection of symptoms associated with HPA axis dysfunction has been referred to as “adrenal fatigue”, however this term is misleading because it inaccurately implies that the adrenal glands become tired or worn out.
Although adrenal hormone production does become altered when we are under chronic stress, these changes are not due to adrenal malfunction or exhaustion. What actually happens in HPA axis dysfunction, is structural and functional changes in the brain, which is an adaptation to chronic stress over time. The brain dials down it’s signaling to the adrenals preventing excess stress hormones from being released. It is thought that this is a protective mechanism when the body has been exposed to excess stress hormones, like cortisol and adrenaline, for a prolonged time.
It is at this point when symptoms of exhaustion and burnout set in. Essentially, your body’s ability to deal with stress becomes compromised.
Some signs and symptoms include:

- Low energy
- Getting sick often, chronic infections
- Slow recovery from illness
- Difficulty concentrating
- Poor memory
- Depression & anxiety
- Cravings for caffeine, sugar, salt
- Feeling tired upon waking
- Feeling more alert in evening
- Sleep disturbances, insomnia
- Increased aches & pains
- Low blood pressure
- Low sex drive
- Irritability, feeling “stressed-out”
- Allergies, hives
People with HPA dysfunction wake up tired in the morning, and feel like they need a nap in the afternoon. But then at night, have trouble sleeping.
A Healthy HPA Axis Influences Overall Health
Having a healthy functioning HPA axis is important for our overall health as it interacts with every other system in the body as well as influences a wide range of chronic diseases.
Chronic stress keeps the HPA axis constantly activated which takes a toll on the entire endocrine system, resulting in numerous health consequences. When cortisol is in excess blood sugar is elevated, which can lead to insulin resistance over time, increasing the risk for diabetes. Blood pressure is elevated, which can lead to cardiovascular conditions. Thyroid hormones are down-regulated, which affects metabolism. Digestive functions slow down, impacting nutrient absorption. Circadian rhythm is also disrupted.
Once the stress response system becomes dysregulated, the body becomes less efficient at responding to stress.
How Natural Medicine Can Help the HPA Axis
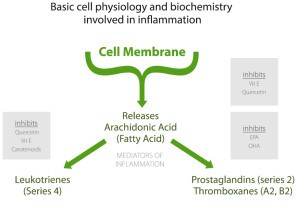
In natural medicine, the goal is to identify and address the root causes of stress that are triggering the hypothalamus to dial back its signaling to the adrenals, so that the stress-induced inflammation can be decreased.
Since multiple factors are at play, the goal is to look for the root cause. Is it blood sugar imbalance? A food intolerance? Is there an infection? Is it emotions?
Reducing stressors and improving the stress response system involves identifying which various root causes are triggering your specific HPA axis dysfunction, as these differ from person to person. It is also important to build up metabolic reserves with nutrients that become depleted with stress and that are needed to produce stress hormones.
Lifestyle, nutrition, and supplement strategies addressing inflammation, blood sugar dysregulation, circadian disruption, as well as factors affecting mood and emotional stress will not only improve the stress response system thus strengthening your resilience to stress, but also lead to overall better health and disease prevention.
While there are numerous ways to support the HPA axis, the following tips can be helpful:
- Eat an anti-inflammatory diet that includes a variety of colorful fruits & vegetables, essential fatty acids, and quality protein.
- Limit caffeine, alcohol, refined sugar and processed foods.
- Maintain proper hydration
- Eat a regular pattern of meals. Skipping meals creates blood sugar imbalance.
- Establish a consistent sleep routine by striving for 7-9 hours of sleep per night in darkness.
- Engage in regular exercise that is not overly vigorous. Strength training or yoga are excellent options.
The following types of supplements have been shown to support HPA axis function. Choosing the appropriate ones depends on the specific areas of stress an individual is experiencing, which is best assessed by a healthcare practitioner.
- Vitamins – vitamin C, B vitamins
- Minerals – magnesium, zinc
- Precursors needed for neurotransmitter synthesis
- Adaptogens – herbs that help the body adapt to stress and bring balance to the body
Try the Naturopathic Approach
References:
Guilliams, T. G. (2015). The role of stress and the HPA axis in chronic disease management. Point Institute, Stevens point (WI), 80.
McEwen, B. S. (2007). Physiology and neurobiology of stress and adaptation: central role of the brain. Physiological reviews, 87(3), 873-904.
McEwen, B. S. (2006). Protective and damaging effects of stress mediators: central role of the brain. Dialogues in clinical neuroscience, 8(4), 367.
Yaribeygi, H., Panahi, Y., Sahraei, H., Johnston, T. P., & Sahebkar, A. (2017). The impact of stress on body function: A review. EXCLI journal, 16, 1057.
